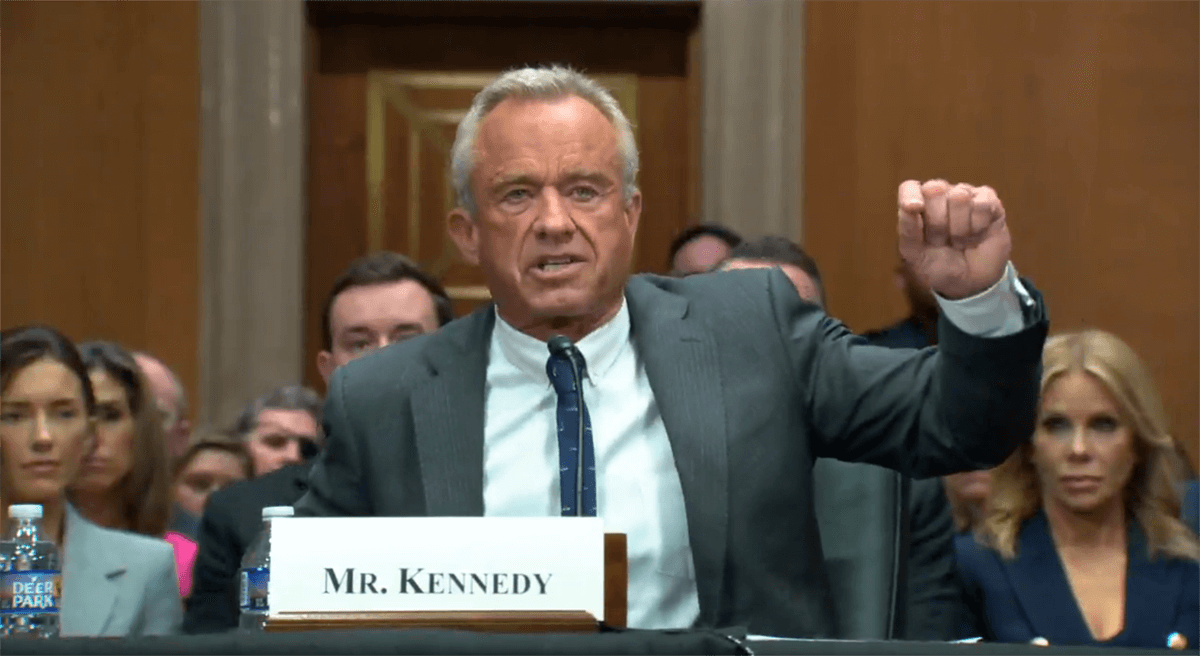
In a significant shake-up within the U.S. Department of Health and Human Services (HHS), Secretary Robert F. Kennedy Jr. has embarked on a major restructuring effort that includes the dissolution of several offices, notably the Office of Infectious Disease and HIV/AIDS Policy (OIDP). This move, announced on Friday, is part of a broader strategy to streamline operations within HHS under the Trump administration, aiming for a more efficient and consolidated approach to public health services.
The OIDP, a critical component of the National Vaccine Program, has been instrumental in coordinating vaccine development, safety, and accessibility efforts across federal agencies. Its elimination, coupled with the announcement of an additional 10,000 employee layoffs at HHS, marks a significant shift in the federal government's role in vaccine initiatives. This follows an earlier reduction of 10,000 workers since the inception of the Trump administration, as reported by CBS News.
This restructuring aligns with the administration's goal to consolidate public health services under a newly established entity, the Administration for a Healthy America (AHA). The AHA is set to absorb responsibilities previously managed by OIDP and other public health offices, including the Substance Abuse and Mental Health Services Administration and the Health Resources and Services Administration. According to an HHS fact sheet, this consolidation represents a fundamental transformation in the operational dynamics of HHS, with an emphasis on efficiency and streamlined services.
Kennedy's aides have indicated that the implementation timeline for the AHA is aggressive, with plans to launch the new agency within the next ten days. This rapid timeline suggests that the administration is committed to swiftly enacting its vision for a reorganized HHS.
The dissolution of OIDP and subsequent restructuring under the AHA raise questions about the future of federal vaccine policy and advocacy. During the Biden administration, OIDP played a pivotal role in public health campaigns, including efforts to combat vaccine hesitancy among parents. With the office no longer in operation, it remains to be seen how these initiatives will be addressed moving forward.
Critics of the restructuring argue that the elimination of OIDP could weaken federal vaccine promotion efforts, shifting more responsibility to states and private organizations. However, supporters contend that consolidating public health agencies under the AHA will lead to improved efficiency and effectiveness in managing health programs.
As the Trump administration moves forward with its plans, the impact of these changes on U.S. public health policy and vaccine advocacy efforts will become clearer. The restructuring represents a significant departure from previous approaches to managing federal health services, signaling a new era in the government's role in public health.