Scientists at the Okinawa Institute of Science and Technology have achieved a significant milestone in Alzheimer's research, successfully reversing memory and learning deficits in mice with disease symptoms. The breakthrough centers on a synthetic peptide called PHDP5 that targets a specific protein interaction responsible for brain cell communication breakdown.
Revolutionary Delivery Method Shows Promise
The research team, led by Professor Emeritus Tomoyuki Takahashi, developed a novel approach using intranasal delivery to bypass the blood-brain barrier. This method allows the therapeutic peptide to reach brain tissue directly without requiring invasive procedures or complex pharmaceutical preparations.
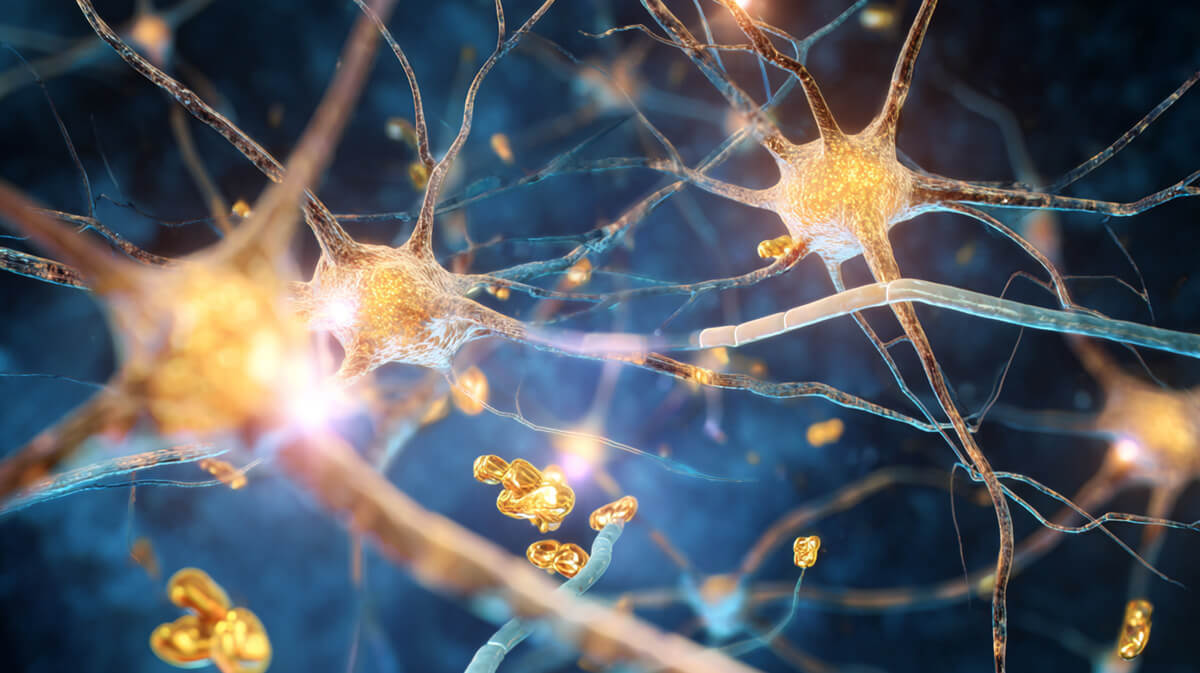
The peptide works by blocking harmful interactions between tau proteins and dynamin, an enzyme essential for healthy cell signaling. In Alzheimer's disease, tau proteins hijack dynamin, disrupting the vital communication links between brain cells called synapses.
"The peptide specifically targets the pathological interaction while preserving normal cellular functions," according to the research published in Brain Research and eLife journals. This precision approach represents a departure from broader pharmaceutical interventions that often produce significant side effects.
Measurable Cognitive Restoration Achieved
Testing involved transgenic mice engineered to develop Alzheimer's-like symptoms. Researchers used the Morris Water Maze, a standard behavioral assessment that measures spatial learning and memory capabilities in laboratory animals.
Treated mice demonstrated cognitive abilities comparable to healthy control animals. The improvement wasn't marginal—researchers observed substantial restoration of learning capacity and memory formation. These results suggest the treatment doesn't merely slow decline but actively reverses existing damage.
The study employed rigorous scientific controls, including scrambled peptide comparisons and double-blind testing protocols. Multiple mouse strains were tested to ensure reproducibility across different genetic backgrounds associated with Alzheimer's pathology.
Understanding the Tau-Dynamin Connection
The research builds on decades of investigation into tau protein behavior in neurodegenerative diseases. Unlike approaches targeting amyloid plaques, this work focuses on tau's role in disrupting synaptic function—the fundamental mechanism by which brain cells communicate.
When tau proteins over-assemble into microtubules, they sequester dynamin away from its normal function in synaptic vesicle recycling. This process essentially starves synapses of the molecular machinery needed for neurotransmitter release and uptake.
The PHDP5 peptide, composed of just 12 amino acids, acts as a competitive inhibitor. It prevents tau from binding to dynamin while allowing normal cellular processes to continue uninterrupted. This targeted intervention addresses a root cause rather than managing symptoms.
Peer Review and Scientific Validation
The research underwent extensive peer review through two established journals. The initial 2022 eLife publication established the theoretical framework and mechanism of action. The 2024 Brain Research paper documented successful therapeutic intervention in living animals.
OIST has secured patent protection for the technology and actively seeks pharmaceutical partnerships through their innovation division. The institute maintains extensive neuroscience research capabilities across multiple specialized units, lending credibility to the findings.
The work has accumulated over 20 citations in scientific literature, indicating recognition within the research community. However, coverage patterns suggest cautious optimism rather than revolutionary excitement among mainstream scientific publications.
Clinical Translation Challenges Ahead
Moving from successful mouse studies to human trials presents substantial challenges. The blood-brain barrier functions differently between species, and what works in laboratory animals doesn't always translate to human physiology.
Regulatory approval processes for neurological treatments are particularly stringent due to the brain's sensitivity and limited regenerative capacity. The FDA typically requires extensive safety data before authorizing human testing of novel therapeutic approaches.
Manufacturing and standardization of peptide therapies also present technical hurdles. Ensuring consistent potency and purity at commercial scales requires sophisticated production facilities and quality control systems.
Broader Research Context
Intranasal peptide delivery for neurodegeneration represents an active area of investigation across multiple institutions. The OIST approach contributes to this growing field while building on established understanding of tau pathology.
Several pharmaceutical companies are pursuing similar strategies targeting different aspects of tau protein dysfunction. This parallel development suggests multiple pathways may ultimately prove necessary for comprehensive treatment.
The research occurs amid ongoing debates about Alzheimer's treatment approaches. Recent controversies surrounding amyloid-focused therapies have intensified interest in alternative targets like tau proteins and synaptic dysfunction.
Timeline and Next Steps
Professor Takahashi recently retired after a 50-year career, but the research continues under Dr. Zacharie Taoufiq's Synapse Biology Unit and Dr. Chia-Jung Chang's Neural Computation Unit. This institutional continuity suggests sustained commitment to advancing the work.
The team has not announced specific timelines for human trials, reflecting the cautious approach typical of early-stage therapeutic development. Industry experts estimate several years of additional preclinical work before regulatory submissions become feasible.
Current efforts focus on optimizing peptide formulation, determining optimal dosing regimens, and conducting long-term safety assessments in animal models. These foundational steps are essential for eventual clinical translation.
The research represents meaningful progress in understanding tau-based therapeutic approaches for Alzheimer's disease. While significant challenges remain before human applications become reality, the work demonstrates that targeted intervention in specific disease mechanisms can produce measurable cognitive improvements in laboratory settings.
Sources: Okinawa Institute of Science and Technology, eLife journal, Brain Research journal, EurekAlert, ScienceDaily, Medical News Today, PubMed